What The Fact?
Are greed and capitalism the reason for successful vaccines?
Photo: U.S. Army Soldier combat medics and administrative assistants administer the COVID-19 vaccine at Delta College, University City, Michigan, on March 6, 2021. Photo by David Kujawa/U.S. Air National Guard via Fickr CC-BY-NC
The Claim
In March 2021, on a private call with Conservative MPs, British Prime Minister Boris Johnson claimed
“The reason we have the vaccine success is because of capitalism, because of greed my friends.”
The prime minister made the comment during a Zoom meeting just before Easter, with a group known as the 1922 Committee, consisting of Tory backbenchers. Johnson lauded the fact that over 28 million people had had their first vaccine dose in the UK, claiming that the success of the Covid-19 vaccination program was a direct result of greed and capitalism.
The comments were soon met with criticism when they were leaked to the public, reviving the debate about public or private ownership rights and public health. Does the source of investment to develop, produce and distribute vaccines impact on public ownership or private industry (big pharma) rights? Others on the call sought to give context to the prime minister’s words, saying that the comments were made in relation to the rapid, safe creation of vaccines by big pharmaceutical firms.
So, if corporate greed was the reason big pharmaceutical companies managed to produce vaccines in record time, this suggests that private, rather than taxpayers through public funds, were the reason for vaccine success.
The Verdict

The claim is rated false (inaccurate based on the best evidence publicly available at this time), on a number of levels:
- Covid-19 vaccine technologies were built on a body of existing research that was largely publicly funded.
- Only $9.8 billion of $172.7 billion of known funding for vaccine R&D since January 2020 was paid by private donors.
- The EU and US alone spent over $38.87 billion on Advanced Purchase Agreements, which accelerated the creation of successful Covid-19 vaccines.
The Evidence
Just because the companies that developed the vaccines are private pharmaceutical companies, does not mean that the research and development (R&D) was privately funded.
Public funding for vaccines can by divided into 3 broad categories:
(1) pre-pandemic funding for general vaccine research,
(2) funding for vaccine research, development and manufacturing in response to the Covid-19 pandemic, and
(3) Advanced Purchase Agreements (APAs), where governments committed to buying a certain number of doses at a fixed price before a vaccine was fully developed.
1. Pre-pandemic funding for research
It is necessary to take into account the millions of dollars in public money invested in general vaccine research in the years leading up to the Covid-19 pandemic.
From the year 2000 onwards, $18.3 billion was spent on HIV vaccine research in the US, 80% of which was paid for by the US federal government. Current vaccine successes would not have been possible without the findings of these research programs. In the same period, the Biomedical Research and Development Authority (BARDA) invested hundreds of millions in the mRNA platform for vaccine development, which underpinned the Pfizer and Moderna technologies.
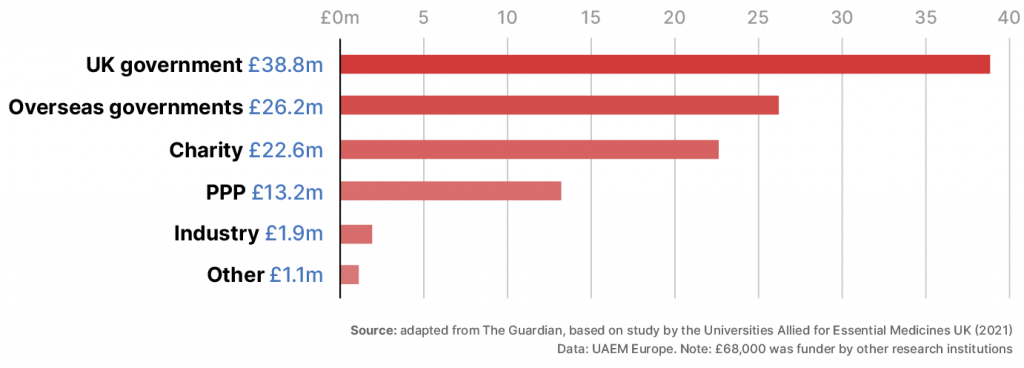
In Johnson’s own country, the development of the Oxford/AstraZeneca vaccine was at least 97% funded by taxpayers or charitable trusts, according to a study by Universities Allied for Essential Medicines UK. The study identifies the source of millions of pounds in research grants from the year 2000 onwards for published work that formed the basis of the vaccine technology, as well as funding for the vaccine itself.
Taxpayers and charitable foundations provided the majority of the funding for Oxford/AstraZeneca vaccine identified by FOIs
2. Funding for Covid-19 vaccine research, development and manufacturing
Since Covid-19 pandemic began, governments have invested in vaccine development by supporting pre-clinical studies, covering the costs of human testing, and ensuring sufficient manufacturing capacity.
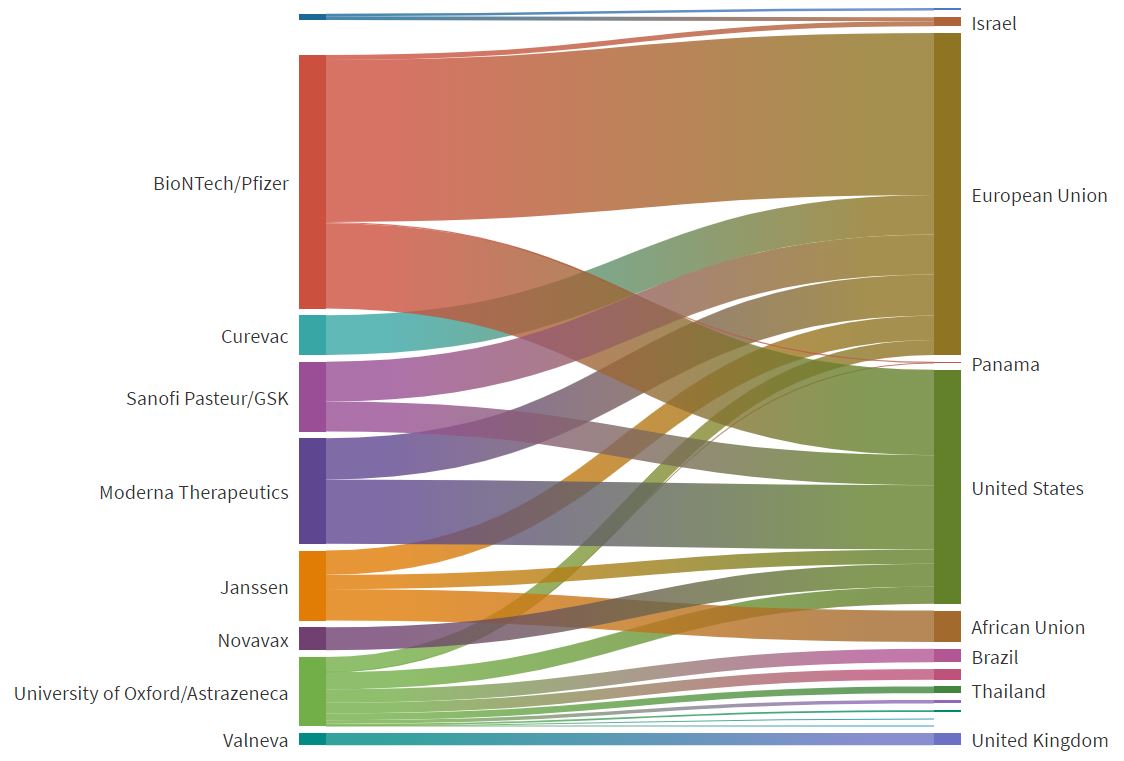
By March 2021, 96 COVID-19 vaccines were at various stages of clinical development.
Graphic: The Knowledge Network on Innovation and Access to Medicines (July 8, 2021)
Public data collected by Devex reports that funding for vaccine development since January 2020 totals $172.7 billion, over 90% of which was public. Multilateral organisations were major donors, with the International Monetary Fund donating $50 billion, the World Bank donating roughly $44 billion and the European Union donating over $25 billion.
National donors were also instrumental, donating a total of over $40 billion. The US and Germany were by far the largest investors in vaccine R&D, followed by a relatively small number of other high-income countries.
Estimates of US government spending on vaccine development range between $18 billion and $23 billion. The Congressional Budget Office estimated that the Biomedical Research and Development Authority (BARDA) alone spent $19.3 billion on the development of Covid-19 vaccines. Operation Warp Speed, the US government funding program, is credited with speeding up the development of vaccines, including issuing a $53 million contract to build manufacturing capacity for Moderna Inc. in May.
Globally, private funds were dwarfed by public funds, accounting for only $9.8 billion overall. Interestingly, according to the data, the Hong Kong- made Sinovac was the only vaccine funded mostly privately. The figure below, from the Graduate Institute of International and Development Studies, demonstrates the proportion of public funding. The bottom graph includes APAs, whereas the top graph does not.
Graphic: Source of COVID-19 vaccine research and development investments, by source country, funder type and type of investments
Graphic: The Knowledge Network on Innovation and Access to Medicines, based at the Graduate Institute of International and Development Studies (July 8, 2021)
3. Advanced Purchase Agreements (APAs)
Advanced Purchase Agreements were made by governments the world over to assure pharmaceutical giants that there would be sufficient demand for their products, essentially eliminating market risk and secure priority access.
These contracts were made before the safety and efficacy of the vaccines were affirmed, and provided an additional incentive for pharmaceutical firms to produce vaccines. The US and the EU led APA arrangements: the EU spent over $22.5 billion on APAs, while the US coughed up over $16.37 billion. The graphic below shows the proportion of APA flows from governments to pharmaceutical companies.
Vaccine R&D Funding Flow: Advanced purchase agreements (in millions USD)
To get an idea of the enormity of these purchases: Johnson & Johnson had a $1 billion contract with the US for 100 million doses; Moderna had a contract with the US totalling $4.95 billion for 300 million doses, and Pfizer had a contract worth $5.97 billion with the US, and a contract of $11.34 billion with the EU.
Limits to data collection
It is difficult to get a conclusive figure for private investment in vaccine R&D. Investments from the pharmaceutical industry are likely to be underreported, as the data is not publicly available because many funding arrangements are labelled as ‘confidential’.
It is also possible that governments overstate the impact of their contributions for political gain. Griffin, Armstrong and Bloomberg, in an article in Fortune, argue that US APAs did not fund the Pfizer-BioNTech vaccine as human testing had begun in April, three months before the US signed its contract. Nonetheless, this agreement would reduce market risk, allowing the company to direct all its resources into the manufacturing of the vaccine.
On the flip side, pharmaceutical giants have an incentive to downplay their public funding, to justify profiting from vaccines. The CEO of Pfizer, for example, Albert Bourla, insists the firm avoided government money for vaccine R&D, despite partner BioNTech receiving $445 million from the German government in September 2020.
Conclusion
As reported by Dr Olivier Wouters’ team in medical journal The Lancet, more than two thirds of the world’s doses have been secured by governments representing just one sixth of the world’s population for 2021. Should patents and intellectual property rights be waived and a guaranteed proportion of APAs to include vaccines for low-income countries?
The debate over who owns vaccines in this context rolls on, let alone the stark reality of how the majority of people on the planet will not receive a first dose by the end of the year.
The People’s Vaccine Alliance, a global coalition of health and humanitarian organisations, is calling for a ‘people’s vaccine’ approach, not ‘a profit vaccine’:
Prevent monopolies on vaccine and treatment production by making public funding for research and development conditional on research institutions and pharmaceutical companies freely sharing all information, data, biological material, know-how and intellectual property.”
The public data available at the time of writing shows that the vast majority of funding for the research, development and manufacturing of Covid-19 vaccines was public, indicating that private funds were not responsible for successful vaccine creation and distribution. Even if we consider the possible underreporting of private investment, the sheer amount of public funding used to reach the extraordinary achievement of developing Covid-19 vaccines in less than 12 months means that it is incorrect to claim that greed and capitalism are the source of vaccine success.
Verdict
Based on the What The Fact? scales guide, the claim is rated as False – the claim is inaccurate based on the best evidence publicly available at this time.
developmenteducation.ie’s What The Fact? supports the code of principles of the International Fact Checking Network. We check claims by influencers, from local to national to transnational that relate to human rights and international human development.
Transparent fact checking is a powerful instrument of accountability, and we need your help.
Send tips and ideas to facts@developmenteducation.ie
Join the conversation #whatDEfact on Twitter @DevEdIreland and Facebook @DevEdIreland
- Tagged as: Companies, Covid-19, pharma, pharmaceutical, vaccines
Sources
- Griffin, Armstrong and Bloomberg, Germany funded the development of Pfizer’s COVID vaccine—not U.S.’s Operation Warp Speed, Fortune, (10 November, 2020)
- Allegretti and Elgot, Covid: ‘greed’ and capitalism behind vaccine success, Johnson tells MPs, The Guardian (24 March 2021)
- Global Health Centre, COVID-19 Vaccines R&D Investments, Graduate Institute of International and Development Studies (8 July 2021)
- Cornish, Lisa, Funding COVID-19 vaccines: A timeline, Devex (21 August 2020)
- Frank, Dach and Lurie, It Was The Government That Produced COVID-19 Vaccine Success, Health Affairs (14 May 2021)
- Safi, Michael, Oxford/AstraZeneca Covid vaccine research ‘was 97% publicly funded’, The Guardian (15 April 2021)
- Cross et al. Who funded the research behind the Oxford-AstraZeneca COVID-19 vaccine?: Approximating the funding to the University of Oxford for the research and development of the ChAdOx vaccine technology (10 April 2021)
- Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment by Olivier J Wouters, Kenneth C Shadlen, Maximilian Salcher-Konrad, Andrew J Pollard, Heidi J Larson, Yot Teerawattananon, Mark Jit in The Lancet (Feb 12, 2021)
- Has only 1% of the 1.3 billion vaccines injected globally been administered in Africa? by Gina Dorso on developmenteducation.ie